|
775 participants from SPIN were asked to complete UCLA Loneliness Scale-6by Steve Bryson, PhD | February 13, 2024 More conversations, either one on one or in groups via telephone or virtually, along with in-person household activities and conversations, were significantly associated with less loneliness during the COVID-19 pandemic among people with systemic sclerosis (SSc), a study indicates.
Conversations and activities at the beginning of the pandemic didn’t predict loneliness over the following two years, however. The findings suggest “sustained levels of interactions over time were potentially more useful than levels of interactions when the pandemic began,” the researchers wrote in “Moderators of Loneliness Trajectories in People with Systemic Sclerosis During the COVID-19 Pandemic: A SPIN COVID-19 Cohort Longitudinal Study,” which was published in the International Journal of Behavioral Medicine. SSc, or scleroderma, is an autoimmune disorder that affects connective tissue, damaging the skin and possibly the internal organs, including the heart and blood vessels, lungs, stomach, and kidneys. During the COVID-19 pandemic, people with SSc had a higher risk of disease and death due to compromised lung function, overall poor health, and the use of immunosuppressant medications. As a result, many faced long periods of isolation, which may have been worsened by physical limitations, such as fatigue and chronic pain. Such isolation may have induced feelings of loneliness, an unpleasant emotional response often associated with a perceived lack of social relationships that fails to fulfill social needs. A Phase 2 trial will explore effect of AM1476 on skin thickness, lung function by Andrea Lobo, PhD | February 6, 2024 AM1476, AnaMar’s investigational anti-fibrotic medication, has been granted orphan drug status by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for treating scleroderma.
To get this designation, a medication must be intended to treat a life-threatening rare disease that affects fewer than five in 100,000 people in Europe or under 200,000 people in the U.S. The designation provides certain incentives, including regulatory fee reductions and the potential for extensive market exclusivity — seven years in the U.S. and 10 in the European Union — if approved. The company plans a Phase 2 clinical trial to evaluate the treatment in people with scleroderma and interstitial lung disease (ILD), a group of diseases marked by lung scarring. The study will evaluate AM1476’s effects on skin thickness and lung function in 60 patients with diffuse cutaneous scleroderma and ILD over a year. “This is a significant milestone and underscores the significant unmet need for novel medicines to prevent, heal, and slow organ scarring from fibrotic diseases, which are often progressive and can have a poor prognosis,” Ulf Ljungberg, PhD, AnaMar’s CEO, said in a company press release. Scleroderma, also known as systemic sclerosis, is marked by inflammation and fibrosis, or uncontrolled tissue hardening and scarring, in the skin and even the heart, kidneys, and lungs. Up to 80% of people with SSc may develop ILD, which leads to reduced lung function and breathing problems. Spike promotes infiltration of pro-inflammatory cells in mouse model by Andrea Lobo, PhD | January 30, 2024 SARS-CoV-2, the virus that causes COVID-19, may accelerate the development and progression of systemic sclerosis (SSc) through fibrosis (scarring), inflammation, autoantibody production, and blood vessel damage.
That’s according to a study in South Korea that shows the SARS-CoV-2 spike protein that’s required for the virus to infect human cells promotes the infiltration of pro-inflammatory cells in the skin and lung tissue of an SSc mouse model. The study, “SARS-CoV-2 spike protein accelerates systemic sclerosis by increasing inflammatory cytokines, Th17 cells, and fibrosis,” was published in the Journal of Inflammation. SSc is an autoimmune disease that features scar tissue accumulating in the skin and potentially the internal organs, including the heart, kidney, lungs, and digestive tract. The disease is thought to develop due to excessive scarring, autoantibodies being produced that mistakenly attack healthy tissues, and damage to small blood vessels. COVID-19 induces the overactivation of immune cells, inflammation, autoantibody production, and bleeding disorders, similar to mechanisms in SSc and other autoimmune diseases. “While there is a single case report suggesting an association between COVID-19 and SSc, the effects of COVID-19 on SSc are not yet fully understood,” wrote the researchers who used human embryonic kidney cells that were manipulated to produce the SARS-CoV-2 spike protein and the ACE2 receptor, a protein to which the virus binds to enter cells. The spike protein is also known to induce fibrosis, the investigators said. Its presence significantly increased the activity of proteins associated with fibrosis, namely alpha-SMA and Col1a1. Patients in interview study talk of the various life changes they have to confront by Marisa Wexler, MS | January 23, 2024 Living with scleroderma requires adapting to changes in a woman’s sense of self, but practicing gratitude and accepting change can help patients reclaim themselves, a study aiming for a “grounded theory” of identify management reports.
Its scientists said these findings may lay the groundwork for future studies aiming to develop interventions to help people with scleroderma hold on to their sense of self while navigating life with the progressive disease. The study, “Process of Maintaining Self in Individuals Living With Systemic Sclerosis: A Grounded Theory Study of American Women,” was published in the Western Journal of Nursing Research. Flow-mediated dilation 'helpful tool in the overall assessment of vascular injury' by Lindsey Shapiro, PhD | January 16, 2024 A non-invasive technique called flow-mediated dilation (FMD) could be useful for monitoring blood vessel alterations in people with systemic sclerosis (SSc) and predicting the likelihood of certain blood flow (vascular) complications, a study has found.
The test findings show distinct differences between SSc patients and healthy people, and were more altered in SSc patients who had been living with the disease longer and had certain vascular symptoms, including pulmonary arterial hypertension (PAH). This correlated well with the degree of damage seen in other tests of vascular damage as well as blood biomarkers of the endothelial cell dysfunction thought to drive blood vessel changes in SSc. The study, “Flow Mediated Dilation in Systemic Sclerosis: Association with clinical findings, capillaroscopic patterns and endothelial circulating markers,” was published in Vascular Pharmacology. Endothelial dysfunction drives blood vessel damage, blood flow changes Alterations to the endothelial cells that line blood vessels — called endothelial dysfunction — drive blood vessel damage and blood flow changes in SSc. As a result, patients may experience certain vascular complications such as Raynaud’s phenomenon, PAH, or digital ulcers. Small blood vessels (i.e. capillaries) as well as larger vessels (i.e. veins and arteries) in patients may be affected, known as microvascular and macrovascular damage, respectively. Microvascular damage is more common and better characterized. These changes can be assessed using a technique called nailfold video-capillaroscopy (NVC), where the capillaries under the skin near the fingernail beds are visualized under a microscope. A method for detecting macrovascular damage is not as well established. FMD, which looks at an artery’s diameter in response to blood flow restriction, could be one way to do this, but it is not yet widely used in clinical practice. Cabaletta Bio developing CAR T-cell therapy for other autoimmune conditions by Marisa Wexler, MS | January 9, 2024 The U.S. Food and Drug Administration (FDA) has granted fast track designation to the cell therapy CABA-201 for organ dysfunction in people with scleroderma.
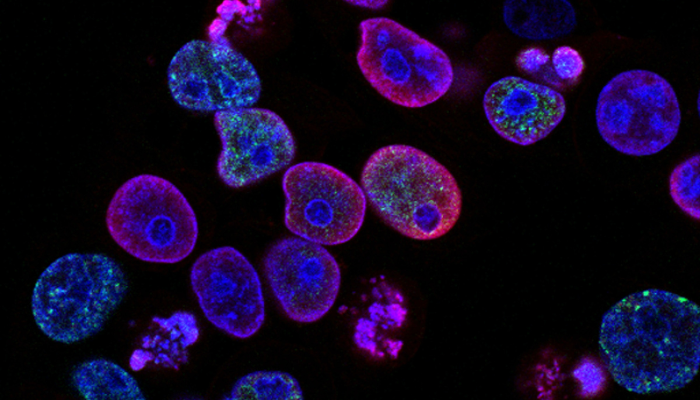
The agency also granted CABA-201 fast track status to reduce disease activity in people with dermatomyositis, another rare disorder that’s marked by muscle weakness and skin rash. The FDA had previously given CABA-201 fast track designation as a potential treatment for lupus. “The additional Fast Track Designations for CABA-201 … provide the opportunity for expedited development and review of CABA-201 for the treatment of these autoimmune indications where there is a significant unmet need, despite currently available therapies,” David Chang, MD, chief medical officer at Cabaletta Bio, which is developing CABA-201, said in a company press release. Higher cholesterol linked to lower risk of scleroderma in South Korean study by Margarida Maia, PhD | January 2, 2024  People with more circulating cholesterol — a type of lipid (fat) that plays an important role in the body — may be at a lower risk of developing systemic sclerosis (SSc), according to a study of nearly 10 million people living in South Korea.
Based on these findings, researchers suggest that a person’s lipid levels, which can be profiled from a blood test, may tell how likely that person is to develop SSc, which could help in early diagnosis. The study, “Association Between Lipid Profile and Risk of Incident Systemic Sclerosis: A Nationwide Population-Based Study,” was published in the journal Clinical Epidemiology. Raynaud's phenomenon is a common systemic sclerosis symptom by Steve Bryson, PhD Elevated activity of a blood-clotting protein called Factor XIII (FXIII) in the bloodstream of adults with systemic sclerosis (SSc) is tied to the presence of Raynaud’s phenomenon, a common SSc symptom, a small study suggests.
While most study participants had FXIII activity levels within the normal range, “patients with higher FXIII activity are more likely to have circulatory disorders in their hands,” the researchers noted. The study, “Factor XIII and Endothelial Dysfunction in Patients with Systemic Sclerosis,” was published in the journal Hämostaseologie. In survey, caregivers highlight key barriers to diagnosis, treatment by Steve Bryson, PhD Caregivers of children with juvenile scleroderma cited a lack of knowledge about the rare disease within the medical community as the primary barrier to a proper diagnosis and treatment, according to a new survey study.
For more than a quarter of the children, it took more than a year from the first symptoms to get a correct diagnosis. Misdiagnoses — ranging from allergies to eczema to a congenital overgrowth disorder — were commonly reported. Other major hurdles reported by almost all respondents included finding reliable information about scleroderma — especially regarding pediatric patients — juggling work and the child’s healthcare needs, side effects of medications, and balancing care and school. “Identifying key care barriers will help direct efforts to address needs, reduce disparities in care, and improve patient outcomes,” the researchers wrote, noting that delays in diagnosis and treatment “have been associated with more persistent disease activity, higher damage scores, and higher relapse rates.” The survey study, “Barriers to care in juvenile localized and systemic scleroderma: an exploratory survey study of caregivers’ perspectives,” was published in the journal Pediatric Rheumatology. Wrong diagnosis common for many children with scleroderma Juvenile scleroderma is a rare type of childhood scleroderma. Most cases are characterized by localized hardened patches of skin, particularly on the arms, legs, or trunk (torso). In more severe cases, the disease can affect organs throughout the body — this is known as systemic scleroderma — including the heart, kidneys, and blood vessels. In some children, these symptoms can be life-threatening. Late diagnoses are common, with reported wait times of up to three years. Resulting delays in treatment have been linked to more and lasting disease activity, more tissue and organ damage, and more relapses. The objective of this study, conducted as an online survey, was to investigate the obstacles caregivers encounter when attempting to access specialized care and treatment for children with juvenile scleroderma. “This information could then guide future efforts to develop effective interventions to reduce diagnostic and treatment delays,” the researchers noted. Study targets correlations among SSc patients with different types of lung disease by Andrea Lobo, PhD The degree of skin tightening is associated with changed levels of proteins implicated in inflammation and cell death among systemic sclerosis (SSc) patients with pulmonary involvement, a study in India reports.
The study established protein correlations among SSc patients with different types of lung disease, which might contribute to identifying lung involvement in people with newly diagnosed SSc, the team suggested. “A longitudinal follow up in these patients with assessment of these immunological parameters may be helpful in monitoring the disease,” the researchers wrote. The study, “A comparative study of modulatory interaction between cytokines and apoptotic proteins among Scleroderma patients with and without pulmonary involvement,” was published in the journal Cytokine. SSc is characterized by abnormal scarring of the skin and potentially internal organs, such as the heart, kidney, lungs, and digestive tract. The disease is thought to develop from the combination of immune dysfunction — meaning the activation and recruitment of immune cells and the production of self-targeting antibodies (fibrosis) — and damage to small blood vessels. The most prominent forms of lung involvement in SSc are interstitial lung disease (ILD), a group of conditions characterized by lung inflammation and fibrosis, and pulmonary arterial hypertension (PAH), caused by the narrowing of small blood vessels that transport blood to the lungs. Studies have reported the involvement of proinflammatory and pro-fibrotic signaling molecules called cytokines in SSc. Also implicated in the disease are proteins associated with apoptosis — programmed cell death (as opposed to cell death caused by injury), which can alter immune responses. To investigate the possible correlation between blood cytokines and apoptotic proteins in SSc, researchers in India analyzed 100 treatment-naïve SSc patients, with or without pulmonary involvement, as well as 100 healthy people who served as controls. |
AuthorScleroderma Queensland Support Group Archives
April 2024
Categories
All
|
Scleroderma Association of Queensland
©Scleroderma Association of Queensland. All rights reserved. Website by Grey and Grey.